
Plastic Toxins & Fertility: The Chemical Toll on Global Sperm Counts
Discover how plastic toxins are causing a global fertility crisis. Learn about BPA, phthalates, and their impact on declining sperm counts worldwide.
HEALTH/DISEASEMODERN DISEASESHARSH REALITY
Kim Shin
9/4/20256 min read
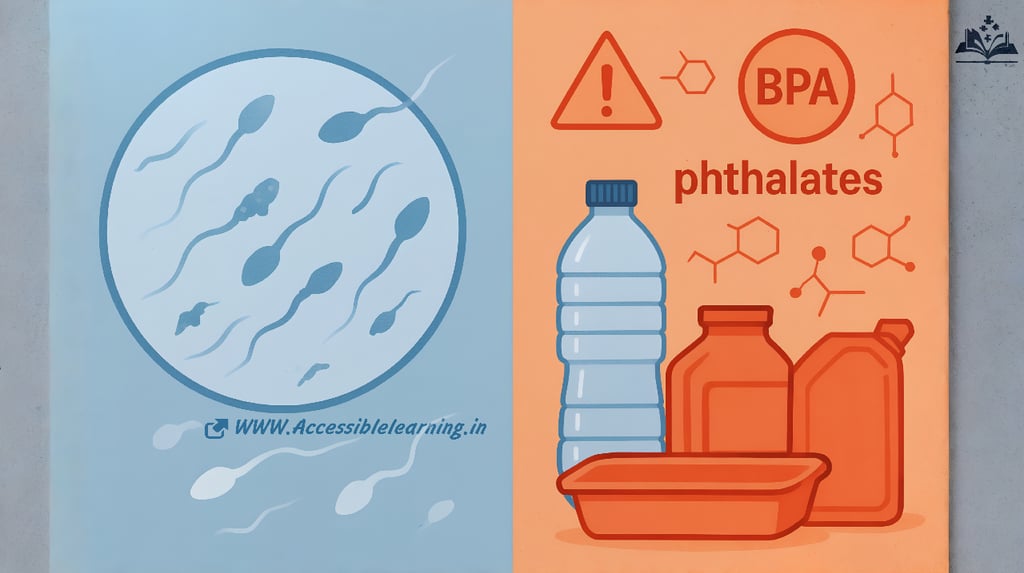

The modern world's dependence on plastic has created an invisible crisis affecting human reproductive health. Over the past five decades, global sperm counts have declined by more than 50%, with plastic-derived chemicals emerging as primary contributors to this alarming trend. This comprehensive examination explores the complex relationship between plastic toxins and fertility, revealing how everyday exposure to these ubiquitous chemicals threatens reproductive health across populations worldwide.
Understanding Plastic Toxins and Their Sources
Primary Chemical Culprits
Plastic products contain numerous chemical additives that can migrate into the environment and human body. The most concerning compounds for reproductive health include bisphenol A (BPA), phthalates, polystyrene derivatives, and per- and polyfluoroalkyl substances (PFAS). These chemicals serve various functions in plastic manufacturing, from increasing flexibility and durability to preventing degradation and enhancing performance characteristics.
BPA, commonly found in polycarbonate plastics and epoxy resins, acts as an endocrine disruptor by mimicking estrogen in the human body. This hormonal interference can significantly impact reproductive function in both men and women. Phthalates, used as plasticizers to increase flexibility in polyvinyl chloride (PVC) products, have demonstrated particularly strong associations with reduced sperm quality and altered hormone levels.
Pathways of Human Exposure
Human exposure to plastic toxins occurs through multiple pathways that make complete avoidance nearly impossible in modern society. Food packaging represents the largest source of exposure, with chemicals leaching from containers, wrapping materials, and processing equipment into consumables. Heating plastic containers or storing acidic foods significantly accelerates this migration process.
Environmental contamination through plastic waste and microplastics presents another major exposure route. These microscopic particles, now detected in drinking water, air, and food chains globally, carry concentrated levels of toxic additives directly into human systems. Indoor air pollution from plastic furnishings, carpets, and building materials creates continuous inhalation exposure, while personal care products and cosmetics containing plastic-derived chemicals contribute through dermal absorption
The Fertility Crisis: Current Research and Statistics
Global Decline in Sperm Quality
Recent meta-analyses examining sperm quality data from 1973 to 2018 reveal a consistent and accelerating decline in sperm concentration, total count, and motility across Western populations. The average sperm concentration has decreased from approximately 101 million per milliliter to 49 million per milliliter over this period, representing a decline of more than 51%. This trend shows no signs of plateauing, with the rate of decline actually accelerating in recent years.
Geographic variations in sperm quality correlate strongly with industrialization levels and plastic consumption patterns. Countries with higher plastic production and consumption demonstrate more pronounced fertility declines, suggesting a direct relationship between chemical exposure and reproductive health outcomes.
Female Reproductive Health Impacts
While sperm quality decline has received significant attention, plastic toxins equally affect female fertility. Exposure to BPA and phthalates has been linked to polycystic ovary syndrome (PCOS), endometriosis, and premature ovarian aging. These chemicals disrupt normal hormonal cycles, affecting ovulation, egg quality, and implantation success rates.
Studies of women undergoing in vitro fertilization (IVF) treatments demonstrate clear associations between higher urinary concentrations of plastic-derived chemicals and reduced success rates. The chemicals appear to affect multiple stages of reproduction, from egg development through early pregnancy maintenance.
Mechanisms of Reproductive Toxicity
Endocrine Disruption Pathways
Plastic chemicals exert their reproductive effects primarily through endocrine disruption mechanisms. These substances can bind to hormone receptors, blocking or mimicking natural hormone signals essential for reproductive function. BPA's ability to bind estrogen receptors disrupts the delicate hormonal balance required for normal reproductive cycles in both sexes.
Phthalates interfere with androgen signaling pathways, reducing testosterone production and affecting the development and function of male reproductive organs. This anti-androgenic activity begins during fetal development and continues throughout life, creating cumulative effects that manifest as reduced fertility in adulthood.
Cellular and Molecular Damage
Beyond hormonal effects, plastic toxins cause direct cellular damage to reproductive tissues. Oxidative stress induced by these chemicals damages sperm DNA, reducing fertilization capacity and increasing the risk of genetic abnormalities in offspring. Similar oxidative damage affects egg cells, contributing to age-related fertility decline and pregnancy complications.
Epigenetic modifications caused by plastic chemical exposure can alter gene expression patterns in reproductive cells, potentially transmitting fertility problems to future generations. These changes affect genes controlling hormone production, cell division, and DNA repair mechanisms essential for healthy reproduction.
Population-Level Health Implications
Demographic and Economic Consequences
The fertility decline associated with plastic toxin exposure extends beyond individual health concerns to create significant demographic and economic challenges. Reduced birth rates in developed nations contribute to aging populations, increased healthcare costs, and economic instability. The medical costs associated with treating infertility continue to rise as more couples require assisted reproductive technologies.
Countries experiencing the steepest fertility declines face potential population collapse scenarios within decades if current trends continue. This demographic shift threatens social security systems, economic growth, and societal stability on a global scale.
Intergenerational Effects
Research increasingly demonstrates that plastic toxin exposure creates intergenerational effects that compound over time. Chemical exposure during pregnancy can program offspring for reduced fertility, creating a cycle of declining reproductive health across generations. These transgenerational effects suggest that current exposure levels may have consequences extending far into the future.
Studies of grandchildren of women exposed to high levels of endocrine-disrupting chemicals reveal continued reproductive health impacts, indicating that the full consequences of our plastic-dependent lifestyle may not be apparent for several generations.

Vulnerable Populations and Exposure Patterns
Occupational and Environmental Justice Considerations
Certain populations face disproportionately high exposure to plastic toxins due to occupational, environmental, and socioeconomic factors. Workers in plastic manufacturing, recycling, and waste management industries experience elevated exposure levels that correlate with higher rates of reproductive health problems.
Communities located near plastic production facilities, waste sites, and recycling centers demonstrate increased rates of fertility problems and reproductive disorders. These environmental justice issues highlight how the burden of plastic pollution falls disproportionately on vulnerable populations with limited resources to avoid exposure.
Critical Windows of Exposure
Timing of exposure significantly influences reproductive outcomes, with certain life stages representing critical windows of vulnerability. Prenatal exposure affects reproductive system development, potentially programming individuals for lifelong fertility challenges. Puberty represents another sensitive period when hormonal disruption can permanently alter reproductive capacity.
Young adults entering their peak reproductive years face particular challenges as they navigate maximum fertility potential while experiencing peak lifetime exposure to plastic chemicals through modern lifestyle choices and consumer products.
Current Regulatory Landscape and Policy Responses
International Regulatory Approaches
Regulatory responses to plastic toxin exposure vary significantly across jurisdictions, creating a patchwork of protection standards that often prove inadequate. The European Union has implemented some of the most stringent controls on endocrine-disrupting chemicals, including restrictions on BPA in food contact materials and certain phthalates in consumer products.
The United States maintains a more fragmented regulatory approach, with different agencies handling various aspects of plastic chemical regulation. This system creates gaps in protection and allows continued use of chemicals banned elsewhere. International coordination remains limited, despite the global nature of plastic pollution and its health effects.
Challenges in Chemical Assessment
Traditional toxicological testing methods often fail to capture the subtle endocrine-disrupting effects of plastic chemicals, particularly at low doses and over extended periods. Regulatory agencies struggle to establish safe exposure levels for chemicals that may have no safe threshold, especially when considering cumulative exposure to multiple chemicals simultaneously.
The lengthy timeline between exposure and reproductive health outcomes complicates regulatory decision-making, as definitive proof of causation may take decades to establish while exposure continues to increase across populations.
Prevention and Mitigation Strategies
Individual Risk Reduction Approaches
While complete avoidance of plastic toxins remains impossible in modern society, individuals can significantly reduce their exposure through targeted lifestyle modifications. Choosing glass or stainless steel containers for food storage eliminates a major source of chemical migration, particularly when combined with avoiding heating food in plastic containers.
Reading product labels and selecting personal care products free from phthalates and other harmful chemicals reduces daily exposure loads. Supporting organic food production and choosing minimally processed foods helps avoid chemicals used in conventional agriculture and food processing.
Institutional and Policy Solutions
Comprehensive solutions to the plastic toxin crisis require coordinated action across multiple sectors and governance levels. Healthcare systems must improve screening and monitoring for plastic chemical exposure, particularly among vulnerable populations and those seeking fertility treatments.
Educational institutions can implement policies reducing plastic use in food service and learning environments while incorporating reproductive health education that addresses environmental factors. Workplace safety regulations must evolve to better protect workers from chemical exposures that affect reproductive health.

Future Research Directions and Emerging Concerns
Advanced Detection and Monitoring Technologies
Emerging analytical techniques enable more precise measurement of plastic chemical exposure and biological effects, providing opportunities for better understanding dose-response relationships and identifying particularly harmful exposure patterns. Biomonitoring programs can track population-level exposure trends and evaluate the effectiveness of intervention strategies.
Research into the health effects of microplastics and nanoplastics represents a rapidly evolving field with significant implications for reproductive health. These particles may transport chemicals more efficiently into tissues and organs, potentially amplifying toxic effects.
Innovative Treatment and Intervention Approaches
Scientific advances in understanding the mechanisms of plastic toxin effects open possibilities for therapeutic interventions that could mitigate damage or restore reproductive function. Antioxidant therapies, hormone replacement protocols, and genetic interventions may help address some consequences of chemical exposure.
Research into the reversibility of reproductive effects provides hope for individuals already exposed to high levels of plastic chemicals. Understanding which effects are permanent versus recoverable informs both treatment approaches and prevention strategies.
The relationship between plastic toxins and fertility represents one of the most significant public health challenges of the modern era. The evidence linking plastic chemical exposure to declining sperm counts and broader reproductive health problems continues to strengthen, while exposure levels increase globally through continued plastic production and inadequate waste management.
Addressing this crisis requires unprecedented cooperation between researchers, policymakers, industry, and individuals to reduce exposure, develop safer alternatives, and protect reproductive health for current and future generations. The stakes could not be higher, as the continuation of human reproductive capacity depends on our collective response to this chemical threat.
The time for action is now. The fertility crisis linked to plastic toxins demands immediate attention and comprehensive solutions that prioritize reproductive health over chemical convenience. Only through coordinated global action can we hope to reverse these troubling trends and secure a fertile future for humanity.
Subscribe To Our Newsletter
All © Copyright reserved by Accessible-Learning Hub
| Terms & Conditions
Knowledge is power. Learn with Us. 📚


