
Bionic Organs and 3D Bioprinting: How Technology Is Changing the Future of Medicine
Explore how bionic organs and 3D bioprinting are transforming modern medicine. Learn how artificial hearts, lab-grown tissues, and regenerative technology could solve organ shortages and change the future of healthcare.
MODERN DISEASESHEALTH/DISEASEAI/FUTURE
Sachin K Chaurasiya
2/19/20267 min read
Human history has always been shaped by medical breakthroughs. Antibiotics changed infection treatment. Vaccines stopped deadly epidemics. Organ transplantation gave new life to patients with failing organs. Today, the next revolution is unfolding through bionic organs and 3D bioprinting, technologies that aim not only to replace damaged organs but also to redesign healthcare itself.
This article explores the science, real-world progress, challenges, ethics, and future of these technologies in detail.
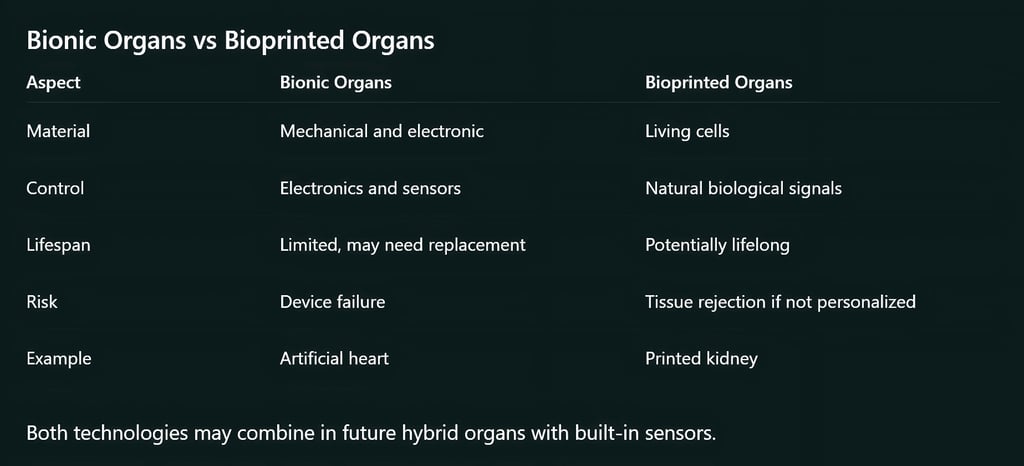
Understanding Bionic Organs
Bionic organs are artificial devices designed to replicate or enhance the function of human organs. They combine electronics, sensors, robotics, and sometimes living tissue. Unlike traditional prosthetics, modern bionic organs interact directly with the nervous system or body chemistry.
Common Types of Bionic Organs
Artificial Heart: Mechanical pumps that circulate blood when the natural heart fails. Some are temporary, others long-term.
Cochlear Implants: Convert sound into electrical signals for the brain. Millions with hearing loss benefit from them.
Bionic Eyes: Retinal implants restore partial vision by stimulating optic nerves.
Bionic Limbs: Controlled by muscle or nerve signals, allowing natural movement.
Artificial Pancreas Systems: Combine glucose sensors and insulin pumps to manage diabetes automatically.
These devices already save lives and improve quality of life worldwide.
Understanding 3D Bioprinting
3D bioprinting uses living cells to create tissues and organs layer by layer. Instead of plastic or metal, printers use bio-ink made from cells and biomaterials.
Key Components of Bioprinting
Bio-ink—Living cells mixed with hydrogels
Scaffold—Temporary structure guiding tissue growth
Bioreactor—Lab chamber where organs mature
Imaging data—MRI or CT scans to model organs
Bioprinting Process
Medical scan of the organ
Computer design of organ structure
Extraction of patient stem cells
Bio-ink preparation
Printing layer by layer
Tissue maturation
Implantation
Organs and Tissues Being Developed
Researchers have successfully created:
Skin grafts for burn victims
Cartilage for nose and ear reconstruction
Blood vessel networks
Bladder tissue
Corneas for vision restoration
Liver tissue patches
Mini organs called organoids are used for drug testing and disease research. Complex organs like kidneys, lungs, and hearts are still under development because they require dense networks of blood vessels and nerves.

The Science Behind These Technologies
1. Stem Cell Biology
Stem cells can transform into any tissue type. They are often taken from the patient, reducing rejection risk.
2. Biomaterials Engineering
Hydrogels, collagen scaffolds, and biodegradable polymers help cells grow into real tissue.
3. Artificial Intelligence
AI helps design organ structures, simulate blood flow, and optimize printing patterns.
4. Nanotechnology
Nanoparticles improve tissue strength, oxygen delivery, and drug release.
5. Neural Interfaces
Electrodes connect bionic devices to nerves, allowing natural control.
Real-World Medical Applications
Burn Treatment
Bioprinted skin heals wounds faster and reduces scarring.
Orthopedic Surgery
Printed cartilage repairs joints damaged by injury or arthritis.
Heart Disease
Artificial hearts and printed heart tissue patches help patients survive until transplant.
Diabetes Management
Artificial pancreas systems regulate insulin automatically.
Vision Restoration
Retinal implants and printed corneas offer hope to blind patients.
Drug Testing
Printed tissues allow testing medicines safely without animal trials.
Organ Shortage Crisis and the Promise of Bioprinting
Globally, millions of patients need organ transplants. Donor organs are limited, and waiting lists are long. Bioprinting could:
Eliminate waiting lists
Reduce transplant rejection
Provide personalized organs
Lower long-term healthcare costs
Hospitals may one day print organs on demand using patient cells.
Ethical and Social Issues
These technologies raise important questions.
Access and Cost
Will only wealthy patients benefit first?
Human Enhancement
Should people use artificial organs to improve strength or memory?
Genetic Editing
Is it ethical to modify organs before implantation?
Identity Questions
How many artificial parts can a human have before becoming “enhanced”?
Regulation
Governments must ensure safety without slowing innovation.
Current Challenges
Despite progress, many obstacles remain.
Biological Challenges
Creating full blood vessel networks
Maintaining organ function long-term
Preventing immune reactions
Ensuring nerve connections
Engineering Challenges
Printing microscopic structures
Scaling production
Maintaining sterile environments
Economic Challenges
High research costs
Insurance coverage issues
Manufacturing complexity
Global Research and Leading Organizations
Major universities, hospitals, and biotech companies are investing heavily in these fields. Key research areas include:
Printed heart muscle patches
Synthetic blood vessels
Neural prosthetics
Artificial kidneys
Biohybrid organs
Government agencies in many countries are funding regenerative medicine programs.
Future Possibilities
In the next few decades, medicine may include:
Fully printed hearts and kidneys
Smart organs with health sensors
Organs printed directly inside the body
Replacement tissues for aging
Custom organs grown in hospitals
Some researchers believe organ failure could become a treatable condition like replacing a car part.

Impact on Healthcare Systems
Hospitals
Bioprinting labs may replace transplant waiting lists.
Medical Education
Doctors will train in regenerative medicine and bioengineering.
Insurance Industry
New policies will emerge for artificial organs.
Global Health
Developing countries may benefit once costs drop.
Manufacturing and Supply Chain Challenges
Even after scientists succeed in creating functional organs, manufacturing them at scale is another challenge.
Producing a single bioprinted organ involves specialized labs, sterile environments, trained technicians, and expensive materials. Scaling this into a global healthcare solution requires:
Automated bioprinting factories
Reliable bio-ink production
Quality control systems
Cold-chain transport for living tissues
Pharmaceutical-style manufacturing standards will likely be needed to ensure safety and consistency. In the future, hospitals may partner with centralized bioprinting centers, similar to how blood banks operate today.
Role of Artificial Intelligence in Organ Design
Artificial intelligence is becoming central to both bionic organs and bioprinting. AI systems can analyze thousands of patient scans to create optimized organ shapes. They can simulate blood flow, tissue growth, and nerve response before an organ is even printed.
AI is also used to:
Detect early organ failure through wearable sensors
Adjust artificial pancreas insulin delivery
Improve neural signals in bionic limbs
Monitor organ performance after surgery
This combination of AI and medical engineering is sometimes called intelligent bioengineering, and it may lead to organs that adapt automatically to a patient’s lifestyle.
Training Doctors for the Next Medical Era
Medical education is changing because of these technologies. Future surgeons may need skills in:
Tissue engineering
Robotics and automation
Bioinformatics
Genetic editing basics
Medical device programming
Medical schools are already adding courses in regenerative medicine. Some universities offer dual degrees in medicine and bioengineering to prepare doctors for these new tools.
Environmental Impact of Bioprinting
Healthcare waste is a growing global issue. Surprisingly, bioprinting could reduce environmental damage in some areas.
For example:
Fewer animal trials reduce biological waste
Local printing reduces transport emissions
Custom organs reduce repeated surgeries
However, labs still consume energy and materials, so sustainable manufacturing methods will be important. Researchers are exploring biodegradable scaffolds and eco-friendly biomaterials.
Cultural and Religious Perspectives
Different cultures and religions may view artificial organs differently. Some questions people ask include:
Is replacing organs with machines acceptable?
Does modifying organs change human identity?
Should enhanced organs be allowed?
Many religious scholars have already supported organ transplantation as a life-saving treatment. Similar discussions are happening for bioprinted organs. Public education will play a big role in acceptance.
Legal Questions and Ownership Issues
New technologies often create new legal questions.
For example:
Who owns a bioprinted organ grown from your cells?
Can companies patent printed organs?
Who is responsible if a bionic device fails?
Healthcare laws will need updates to address these issues. Some countries are already creating regulations for regenerative medicine products. Clear legal frameworks will help protect patients and encourage innovation.
Role in Space Medicine and Extreme Environments
Bionic organs and bioprinting are important for future space travel.
Astronauts on long missions cannot rely on organ donation. Portable bioprinters could create tissues during emergencies.
Researchers are studying printing tissues in zero gravity, where cells can grow differently. This research also helps improve organ design on Earth.
These technologies may also help soldiers, disaster victims, and people in remote areas with limited medical access.
Economic Opportunities and New Industries
This field is creating new jobs and industries. Examples include:
Bio-ink manufacturing companies
Medical robotics firms
Tissue engineering labs
AI healthcare startups
Bioprinting equipment manufacturers
Countries investing early in regenerative medicine may lead a major global industry similar to pharmaceuticals or biotechnology.
Psychological Impact on Patients
Receiving a bionic or bioprinted organ is not only a medical event. It is also emotional. Patients may feel:
Gratitude for new life
Fear about device failure
Identity concerns
Adjustment challenges
Hospitals increasingly include counseling and rehabilitation programs to help patients adapt to artificial organs or prosthetics. Human-centered care will remain essential even in high-tech medicine.


What This Means for Humanity
Bionic organs and bioprinting offer hope for patients with heart failure, kidney disease, blindness, diabetes, and severe injuries. They may extend life expectancy and reduce suffering.
More importantly, they represent a shift toward personalized medicine, where treatment is designed for each individual.
Bionic organs and 3D bioprinting are among the most powerful medical innovations of the 21st century. They merge biology with technology to solve one of humanity’s oldest problems: organ failure.
While technical and ethical challenges remain, progress is steady. What once sounded like science fiction is becoming real. The day may come when hospitals print organs on demand, artificial devices restore lost senses, and human health enters a new age of possibility.
FAQ's
Q: How long do bionic organs usually last?
The lifespan depends on the device. Some artificial hearts or prosthetics last 5–10 years, while cochlear implants can work much longer with maintenance. Regular monitoring and occasional upgrades may be needed.
Q: Are bioprinted organs stronger than natural organs?
Bioprinted organs aim to match natural organs, not exceed them. However, future designs may include reinforced biomaterials or smart sensors that improve durability and monitoring.
Q: Can children receive bionic or bioprinted organs?
Yes, in some cases. Cochlear implants and prosthetic limbs are already used for children. Bioprinted organs for children are still under research because growing bodies require organs that can grow too.
Q: Will these technologies eliminate organ rejection completely?
Using a patient’s own cells greatly reduces rejection risk, but it may not remove it entirely. Doctors still monitor patients carefully after implantation.
Q: How expensive are bionic organs and bioprinted tissues?
Currently, they are expensive because of research and manufacturing costs. As technology improves and production scales up, prices are expected to fall, similar to how smartphones became affordable over time.
Q: Can damaged organs repair themselves using bioprinting?
In some cases, yes. Doctors may print small tissue patches instead of full organs. These patches help damaged organs heal faster, especially in heart or liver injuries.
Q: Are there risks of infection with artificial or printed organs?
Yes, as with any surgery. Hospitals use strict sterile procedures, and patients may need antibiotics or monitoring after surgery.
Q: Can bionic organs be upgraded like software or hardware?
Some devices already allow updates. Artificial pancreas systems and neural prosthetics can receive software improvements that enhance performance without surgery.
Q: Will people with artificial organs be able to live normal lives?
Most patients return to normal activities after recovery. Many people with prosthetic limbs, implants, or artificial hearts work, travel, and exercise regularly.
Q: Which organ will likely be fully bioprinted first?
Experts believe kidneys or liver tissue may be printed before complex organs like lungs or hearts because their structure is easier to reproduce.
Q: Are there age limits for receiving these organs?
Eligibility depends on health condition, not just age. Doctors evaluate each patient’s overall health before recommending treatment.
Q: Can lifestyle affect the performance of a bionic organ?
Yes. Diet, exercise, and regular medical checkups still matter. Artificial organs support health but do not replace healthy habits.
Q: Will insurance companies cover these treatments?
Coverage policies vary by country. As these technologies become common and approved, insurance systems are expected to include them.
Q: Can bioprinting help with cosmetic reconstruction?
Yes. Printed cartilage and skin are already used for facial reconstruction after accidents, burns, or cancer surgery.
Q: Could these technologies help aging populations?
Yes. Repairing or replacing aging organs may improve quality of life and reduce long-term medical costs for elderly patients.
Subscribe To Our Newsletter
All © Copyright reserved by Accessible-Learning Hub
| Terms & Conditions
Knowledge is power. Learn with Us. 📚


